Root Canal Treatment

A root canal (also known as endodontic treatment) is a dental procedure performed by a dentist or an endodontist (a specialist in root canal treatment) to treat a tooth that is severely decayed or infected. The goal of the procedure is to save the tooth and prevent the need for extraction. Here’s a breakdown of the process:
1. When is a Root Canal Needed?
A root canal is necessary when the pulp (the soft tissue inside the tooth that contains nerves, blood vessels, and connective tissue) becomes infected or inflamed. This can occur due to:
- Deep cavities that reach the pulp.
- Trauma to the tooth, such as a crack or chip.
- Repeated dental procedures on the same tooth.
- Gum disease that affects the tooth’s roots.
If left untreated, an infection in the pulp can lead to abscesses, tooth pain, and eventually the loss of the tooth. Root canal treatment is designed to remove the infection and save the tooth.
2. The Root Canal Procedure
The root canal process typically requires one or two visits, depending on the complexity of the case. Here’s how it’s done:
Step 1: Initial Examination
- X-rays: The dentist or endodontist will take X-rays to assess the extent of the infection and examine the shape of the tooth’s roots.
- Numbing: Local anesthesia will be administered to numb the area around the tooth and ensure you don’t feel pain during the procedure.
Step 2: Accessing the Pulp
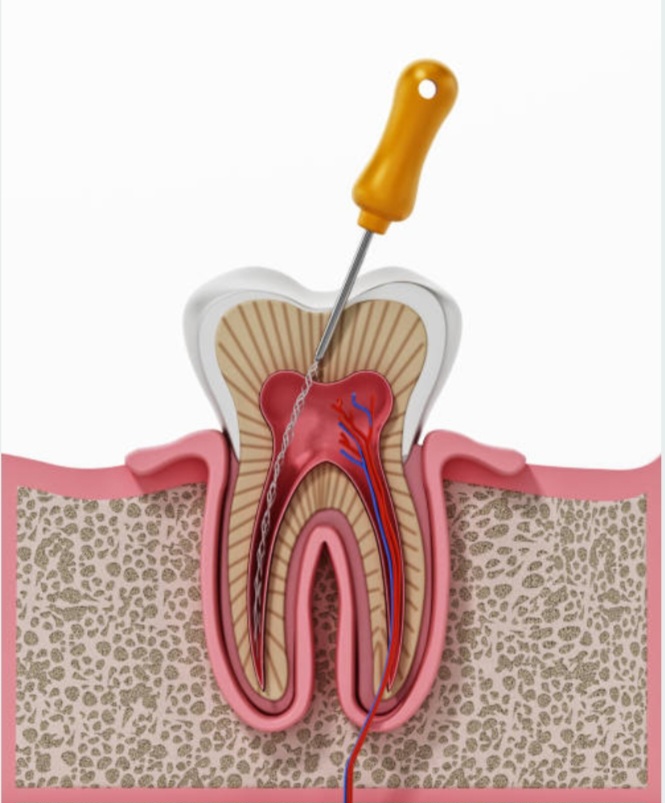
- Opening the Tooth: The dentist will drill a small hole in the top of the tooth (the crown) to access the pulp chamber where the nerves and blood vessels are located.
- Removing the Pulp: Once the pulp is exposed, the dentist will carefully remove the infected or damaged pulp tissue from the inside of the tooth using specialized instruments.
Step 3: Cleaning and Shaping the Root Canals
- Cleaning the Canals: After removing the pulp, the dentist will thoroughly clean and disinfect the hollow root canals to remove any remaining bacteria and debris. This helps prevent further infection.
- Shaping the Canals: The dentist will then shape the canals to prepare them for filling. This step ensures the canals are properly sized and free of infection.
Step 4: Filling the Canals
- Filling Material: Once the canals are clean and shaped, they are filled with a biocompatible material called gutta-percha, which helps seal the canals and prevent future infection.
- Sealing the Access Hole: The dentist will also seal the hole created in the tooth with a temporary or permanent filling to prevent bacteria from entering.
Step 5: Restoration of the Tooth
- Temporary Filling (if necessary): If the root canal is completed in one visit, the dentist may place a temporary filling until the next appointment.
- Crown Placement (if necessary): After the tooth has healed, a dental crown may be placed over the tooth to restore its strength, shape, and function. This is often done for teeth that have significant decay or structural damage. The crown is custom-made to fit over the treated tooth, providing extra protection and making it look natural.
3. After the Root Canal Treatment
- Recovery: After the procedure, you may feel mild discomfort or sensitivity for a few days, which is normal and can be managed with over-the-counter pain relievers.
- Follow-Up Care: You’ll likely need a follow-up appointment to check the tooth’s healing process and possibly place a crown if one is needed.
- Restoration: Once the crown or final restoration is in place, the tooth should function like any other tooth and allow you to chew and speak normally.
4. Benefits of Root Canal Treatment
- Saves the Tooth: The primary benefit is that root canal treatment can save a tooth that would otherwise need to be extracted. By removing the infection, the tooth can be preserved, allowing it to continue functioning properly.
- Relieves Pain: Root canal treatment can eliminate the pain caused by an infected tooth and reduce inflammation.
- Restores Function: After a root canal, the tooth is restored to its natural function, allowing you to chew and speak without discomfort.
5. Common Misconceptions About Root Canals
- Pain: One of the biggest misconceptions is that root canal treatments are painful. In reality, the procedure is done under local anesthesia, so you won’t feel any pain during the treatment. Post-treatment discomfort is usually mild and temporary.
- Success Rate: Root canal treatments have a high success rate, typically 85% to 97%, especially when performed by an experienced dentist or endodontist.
- Tooth Removal: A root canal often allows you to keep your natural tooth, whereas tooth extraction would require a more extensive treatment, such as a dental implant or bridge, to replace the lost tooth.
6. Potential Risks and Complications
- Infection: In rare cases, the infection may not be completely removed, or it could return after treatment. If this happens, the procedure may need to be repeated.
- Cracked Tooth: In some cases, the tooth may crack during or after the procedure, which could affect the success of the root canal.
- Tooth Fracture: Because the tooth becomes more fragile after a root canal, it’s important to restore it with a crown to prevent fractures.
When Is Root Canal Treatment Recommended?
A root canal may be recommended if you experience any of the following symptoms:
- Severe tooth pain, especially when chewing or applying pressure.
- Prolonged sensitivity to hot or cold temperatures.
- Swelling or tenderness in the gums near the affected tooth.
- Darkening of the tooth (sign of internal damage).
- Pimple-like bump on the gums (a sign of an abscess).
Root canal therapy is a highly effective procedure that can save your natural teeth, reduce pain, and restore function, so it’s often considered the best option when infection or damage affects the pulp.